Primary (AL) - light chains
Secondary (AA) - amyloid A
dialysis related amyloidosis - beta 2 microglobulin
age-related - transthyretin
Thursday, May 31, 2018
Friday, May 25, 2018
Neurotransmitters
Serotonin - raphe nucleus
GABA - caudate nucleus (striatum)
norepinephrine - locus ceruleus
acetylcholine - nucleus basalis
dopamine - substantia nigra
GABA - caudate nucleus (striatum)
norepinephrine - locus ceruleus
acetylcholine - nucleus basalis
dopamine - substantia nigra
Monday, May 21, 2018
Review Questions
A 32yo female presents with dyspnea that has gotten progressively worse over the pass few months. Patient's mother experienced similar symptoms and passed away at the age of 50. Genetic analysis reveals that patient has a inactivating mutation in her BMPR2 gene. Which of the following can be used to treat her condition?
A. albuterol
B. bosentan
C. esmolol
D. tamoxifen
E. furosemide
A 26yo male and his wife have been trying to have a child for the past 2 years without any success. Patient has long arms and legs. Blood tests reveal increased FSH and LH, but decreased testosterone and inhibin B. Which of the following is most likely the underlying cause of this patient's complaint?
A. aromatase deficiency
B. Kartagener syndrome
C. 5 alpha reductase deficiency
D. Klinefelter syndrome
E. Marfan syndrome
17yo patient presents to clinic for wellness exam. Upon physical exam, you note that the patient has long limbs. Blood tests reveal elevated homocysteine levels but normal MMA levels. What is this patient at risk for developing?
A. thromboembolic events
B. megaloblastic anemia
C. aortic aneurysm
D. kidney stones
E. recurrent sinus infections
A. albuterol
B. bosentan
C. esmolol
D. tamoxifen
E. furosemide
A 26yo male and his wife have been trying to have a child for the past 2 years without any success. Patient has long arms and legs. Blood tests reveal increased FSH and LH, but decreased testosterone and inhibin B. Which of the following is most likely the underlying cause of this patient's complaint?
A. aromatase deficiency
B. Kartagener syndrome
C. 5 alpha reductase deficiency
D. Klinefelter syndrome
E. Marfan syndrome
17yo patient presents to clinic for wellness exam. Upon physical exam, you note that the patient has long limbs. Blood tests reveal elevated homocysteine levels but normal MMA levels. What is this patient at risk for developing?
A. thromboembolic events
B. megaloblastic anemia
C. aortic aneurysm
D. kidney stones
E. recurrent sinus infections
B
D
A
Friday, April 20, 2018
Pharyngeal Arches, Clefts, and Pouches
For some reason, this doesn't stick in my head unless I draw it all out in one diagram. Hope it helps!
Friday, April 13, 2018
Wednesday, April 4, 2018
Wednesday, March 28, 2018
Heart Murmurs Review
Here's a playlist I made from a few Youtube videos. Heart Murmurs Many thanks to Thinklabs for having so many examples.
Of course we also need to know how they change with maneuvers.
Of course we also need to know how they change with maneuvers.
Monday, March 26, 2018
Microbiology Review
I've attached some charts for microbiology. The yellow boxes are for characteristics that are used to differentiate species. It's also a good idea to add notes on each bug. ^.^
Tuesday, March 6, 2018
Review Questions
A 55 yo patient presents to the ER with subacute endocarditis. Patient’s history was significant for a recent dental procedure. What allows for the organism to bind to damaged heart valves?
A. Pili
B. Dextrans
C. Biofilm
D. TSST-1
E. Protein A
A 6 month old child presents to the clinic with hypotonia. History was significant for ingestion of honey containing spores of a gram (+) rod. What is the mechanism of the toxin produce by this organism?
A) cleavage of SNARE protein inhibiting GABA release
B) damage of cell membranes
C) inhibition of Ach release
D) depolymerization of actin
E) ADP-ribosylation of EF-2
A 10 yo patient presents to the clinic with hematuria. 2 weeks ago, patient had a honey crusted lesion on his face but did not see a physician. Another infection by this organism is pharyngitis. A complication of pharyngitis is a result of antibodies to which portion of the organism?
A. Capsule
B. Protein A
C. Cell wall
D. M protein
E. Erythrogenic toxin
22yo female presents with fatigue for the past few days. Patient became a vegetarian 3 months ago. Blood tests show a decreased MCV but normal ferritin. Patients experienced no other symptoms. What is the cause of RBC damage in this condition?
A) lack of membrane protein that anchors DAF
B) glutamate to valine mutation
C) iron deficiency
D) tetramers of excess globin chains
E) Vitamin B12 deficiency
B
C
D
D
A. Pili
B. Dextrans
C. Biofilm
D. TSST-1
E. Protein A
A 6 month old child presents to the clinic with hypotonia. History was significant for ingestion of honey containing spores of a gram (+) rod. What is the mechanism of the toxin produce by this organism?
A) cleavage of SNARE protein inhibiting GABA release
B) damage of cell membranes
C) inhibition of Ach release
D) depolymerization of actin
E) ADP-ribosylation of EF-2
A 10 yo patient presents to the clinic with hematuria. 2 weeks ago, patient had a honey crusted lesion on his face but did not see a physician. Another infection by this organism is pharyngitis. A complication of pharyngitis is a result of antibodies to which portion of the organism?
A. Capsule
B. Protein A
C. Cell wall
D. M protein
E. Erythrogenic toxin
22yo female presents with fatigue for the past few days. Patient became a vegetarian 3 months ago. Blood tests show a decreased MCV but normal ferritin. Patients experienced no other symptoms. What is the cause of RBC damage in this condition?
A) lack of membrane protein that anchors DAF
B) glutamate to valine mutation
C) iron deficiency
D) tetramers of excess globin chains
E) Vitamin B12 deficiency
B
C
D
D
Saturday, March 3, 2018
Heparin + Warfarin
Why do we give heparin before starting long-term warfarin? Warfarin knocks out Vitamin K epoxide reductase in the liver. This decreases factors 2, 7, 9 and 10. It also decreases protein C and S, which inactivate the coagulation cascade. Although synthesis is stopped, there are still pre-existing factors within the blood. The first ones to decrease are protein C and S. Uh oh...that means you still have coagulation factors floating around and nothing to stop them. This hypercoagulable state could result in skin necrosis! Not to worry. This is why we give heparin to transition the patient onto warfarin therapy. What does heparin do? It binds to antithrombin 3 which inhibits factors 2 and 10.
Vit B12 Deficiency
Vitamin B12 is carries a methyl group from tetrahydrofolate to homocysteine. Homocysteine is then converted in methionine. Without B12, the methyl group cannot be added, increasing levels of homocysteine which makes the blood hypercoagulable.
Thursday, March 1, 2018
Neuro Pathology
Parkinson Disease
Loss of dopaminergic cells in substantia nigra pars compacta (in the basal ganglia) disrupts movement. Classic presentation is tremor, cogwheel rigidity, akinesia, postural instability, and shuffling gait. The condition is associated with Lewy bodies, which are aggregates of α-synuclein.
Huntington Disease
Treatment:
levodopa
carbidopa
entacapone/tolcapone
selegiline
benztropine
bromocriptine, pramipezole, ropinirole
amantadine
Huntington Disease
Huntington disease is an autosomal dominant CAG repeat disorder on chromosome 4. This trinucleotide expansion can result in a gain-of-function that disrupts the normal transcriptional repression by huntingtin. This increases histone deacetylation (so increased transcriptional repression), silencing the genes necessary for neuronal survival. Condition is characterized by chorea, aggression, depression, and dementia.
Alzheimer Disease
APP is usually degraded into A-α but in Alzheimer's, it is degraded into A-β amyloid forms seniles plaques. Neurofibrillary tangles formed from hyperphosphorlyated tau proteins, which are normally in the cytoskeleton.
Treatment:
tetrabenazine, reserpine
haloperidol
Alzheimer Disease
APP is usually degraded into A-α but in Alzheimer's, it is degraded into A-β amyloid forms seniles plaques. Neurofibrillary tangles formed from hyperphosphorlyated tau proteins, which are normally in the cytoskeleton.
Plaques will lead to widespread cortical atrophy, which can present as hydrocephalus ex vacuo. ApoE2 is associated with decreased risk, while ApoE4 is associated with increased risk. Alzheimer is also associated with APP, presenilin-1, and presenilin-2.
Treatment:
memantine
donepezil, galantamine, rivastigmine
Frontotemporal Dementia
Inclusions of hyperphosphorlyated tau proteins form Pick bodies. Frontal lobe involvement results in behavioral changes. Temporal lobe involvement results in aphasia.
Lewy Body Dementia
Lewy bodies are aggregates of α-synuclein. Condition presents as dementia first, then parkinsonian symptoms.
Tuesday, February 27, 2018
Saccular Aneurysms
Why do saccular aneurysms happen at branching points in the Circle of Willis? At these branching points, the wall is weak because the vessel lacks a media layer. Where is the most common site for these berry aneurysms? At the point when the anterior communicating branches from the anterior cerebral artery. You'll probably find something when you do a spinal tap. ;)
Monday, January 22, 2018
Friday, January 19, 2018
Wednesday, January 10, 2018
Sunday, January 7, 2018
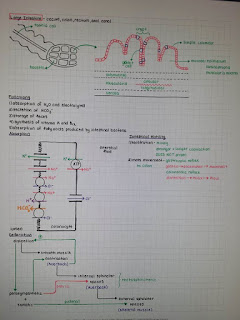
GI Physiology
Upper GI
Stomach
Liver + Gallbladder
Pancreas
Here are my notes. I used lectures from class, Boards and Beyond, some youtube. Hope it helps!
Friday, January 5, 2018
GI Blood Supply
Perforated Ulcers
Ulcers on the lesser curvature of the stomach can cause bleeding from the left gastric artery.
Posterior duodenal ulcers can cause bleeding from the gastroduodenal artery.
Short Gastric Arteries
The short gastric arteries are branches off the splenic artery. They supply the fundus. Unlike other arteries of the stomach, the fundus does not have dual blood supply. Thus it is more vulnerable to ischemia.
Pringle's Maneuver
During an abdominal surgery, you can clamp down on the hepatoduodenal ligament to see if the bleeding stops. If it does, the bleed was from the proper hepatic artery or the portal vein. That's because the hepatoduodenal ligament contains the proper hepatic artery, portal vein, and cystic duct. If the bleeding continues, the bleed is from somewhere else (like the IVC).
SMA Syndrome
The superior mesenteric artery courses over the duodenum. Usually mesenteric fat provides padding, but if there isn't enough fat, the artery can be compresses. This leads to bowel obstruction.
Dual Blood Supply
stomach - celiac trunk and superior mesenteric artery (superior and inferior pancreaticoduodenal arteries)
transverse and descending colon - superior and inferior mesenteric (marginal artery of Drummond)
rectum - inferior mesenteric artery and iliac artery (superior rectal and middle rectal)
Mesenteric Ischemia
-small intestine
-embolism and arterial thrombosis
-venous thrombosis
-under perfusion from shock (affects watershed areas of colon which include splenic flexure and rectosigmoid junction)
-intestinal angina (fear of eating)
-increased WBC, lactate, acidosis
-occult blood in stool
Ischemic Colitis
-colon
Ulcers on the lesser curvature of the stomach can cause bleeding from the left gastric artery.
Posterior duodenal ulcers can cause bleeding from the gastroduodenal artery.
Short Gastric Arteries
The short gastric arteries are branches off the splenic artery. They supply the fundus. Unlike other arteries of the stomach, the fundus does not have dual blood supply. Thus it is more vulnerable to ischemia.
Pringle's Maneuver
During an abdominal surgery, you can clamp down on the hepatoduodenal ligament to see if the bleeding stops. If it does, the bleed was from the proper hepatic artery or the portal vein. That's because the hepatoduodenal ligament contains the proper hepatic artery, portal vein, and cystic duct. If the bleeding continues, the bleed is from somewhere else (like the IVC).
SMA Syndrome
The superior mesenteric artery courses over the duodenum. Usually mesenteric fat provides padding, but if there isn't enough fat, the artery can be compresses. This leads to bowel obstruction.
Dual Blood Supply
stomach - celiac trunk and superior mesenteric artery (superior and inferior pancreaticoduodenal arteries)
transverse and descending colon - superior and inferior mesenteric (marginal artery of Drummond)
rectum - inferior mesenteric artery and iliac artery (superior rectal and middle rectal)
Mesenteric Ischemia
-small intestine
-embolism and arterial thrombosis
-venous thrombosis
-under perfusion from shock (affects watershed areas of colon which include splenic flexure and rectosigmoid junction)
-intestinal angina (fear of eating)
-increased WBC, lactate, acidosis
-occult blood in stool
Ischemic Colitis
-colon
Subscribe to:
Comments (Atom)